Ever wondered why medical billing feels so complicated? From insurance claims to patient billing, it is all tedious and error-ridden. Even small mistakes lead to delayed payment or loss of income to medical professionals.
But what if something could be done to simplify it with the help of technology? That’s where Artificial Intelligence (AI) steps in. AI is revolutionizing medical billing by removing the manual tasks, minimizing the errors, and accelerating the whole process.
The AI In Medical Billing Market size is estimated at USD 4.49 billion in 2025, and is expected to reach USD 12.65 billion by 2030, at a CAGR of 23.01% during the forecast period (2025-2030). The global AI market in healthcare to grow from $20.9 billion in 2024 to $148.4 billion by 2029.
With the non-stop effort of AI, medical billing is speedy, precise, and trouble-free. Let’s find out how AI-based medical billing is changing and improving like never before.
What is AI in Medical Billing And Coding?

Medical billing is necessary in medical administration as it provides proper documentation, billing, and compliance. Medical coding is the process of applying standardized codes to procedures, treatments, and diagnoses, making claims processable and financially addressable in a very simple way.
Apart from billing, accurate coding ensures provision of data-driven decision-making in healthcare, policy making, and overall health quality improvement in healthcare.
Due to growing demand for proficient medical coders, most of the medical centers are not able to fill job openings. As much as 30% of the medical coding jobs remain vacant, decreasing efficiency and accuracy, reports state.
Artificial intelligence medical billing is a smart process of improvement in terms of faster, accurate coding and optimal use of available resources. By integrating AI, the healthcare industry is able to enhance accuracy, ease workload, and optimize revenue cycles without affecting the quality.
How Does AI in Medical Billing and Coding Work?
AI in medical billing and coding is changing by automatically undertaking repetitive tasks, decreasing errors caused by human beings, and making the claim process faster. It decreases the role of human beings only when complexity is introduced, resulting in faster and correct billing.
AI in Medical Billing
AI streamlines medical billing by performing crucial tasks such as data collection, claims submission, and payment tracking. AI reduces errors in claim processing and speeds it up, thus improving overall efficiency.
How AI Streamlines Medical Billing:
- Pre-appointment insurance data verification to avoid claim denial.
- Retrieves and authenticates patient details to ensure all claims are precise.
- Submits claims automatically with notices of potential mistakes in advance.
- Handles rejections and appeals by checking reasons and recommending rectification.
AI in Coding
Medical coding is the most important billing component, and AI adds efficiency by learning from previous coding trends and patient histories. It decreases coding mistakes and maintains up-to-date medical coding changes.
How AI Functions in Coding:
- Recommends the most appropriate codes for procedures according to previous trends.
- Notifies coders when updates or revisions in codes need to be applied.
- Pinpoints patient records that require more examination to avoid billing mistakes.
- Minimizes human errors by sending appropriately processed charts to billing groups.
Through the incorporation of AI in medical billing and coding, medical care providers are able to enhance efficiency, reduce cost, and maximize accuracy, thus improving financial management as well as patient care.
Medical billing has always been a part of healthcare management, with an aim to compensate providers for the services they render. Previously, the process consisted of manual entry of data, paper, and human intervention and thus was not only time-wasting but also error-prone. But that was all before AI-based medical billing, when the process turned out to be more accurate, efficient, and cost-effective.
The following table shows the primary differences between conventional and AI-based medical billing:
| Aspect | Traditional Medical Billing | AI Medical Billing |
| Processing Speed | Data entry takes time for processing claims. | Automates data collection and submission, thus speeding up processing. |
| Accuracy & Error Reduction | Susceptible to human errors, resulting in rejected or delayed claims. | Employs AI algorithms to identify and rectify errors prior to submission. |
| Cost Efficiency | Needs a large workforce, increasing operating costs. | Less labor expense as redundant work is automated. |
| Compliance & Updates | Needs human labor to stay in compliance with regulations. | Automatically stays up to date with compliance regulations, reducing risks. |
| Claim Management & Tracking | Follow-ups must be performed manually, making tracking inefficient. | Real-time claim tracking with real-time correction and analysis. |
| Scalability | More patients and claims result in more employees having to be hired. | Can handle high volumes without additional employees. |
Features of AI in Medical Billing
Medical billing software for artificial intelligence is programmed with core features that automate processes, and improve financial processing in healthcare. Some of the most critical features that facilitate efficiency and accuracy in medical billing are discussed in detail below.
1. Patient Information Management
Managing patient records appropriately is the foundation for all medical billing frameworks. AI offers a means to store and retain patient information, allowing for proper billing and preventing fault areas. The mechanism is easy to manage patient information, such as medical history, insurance, and appointment scheduling, to simplify billing and make it more efficient.
2. Compatibility with Electronic Health Records (EHR)
Simplified information sharing between Electronic Health Records (EHR) makes it possible that medical billing software can retrieve the patient’s information without manual input. This feature ensures that treatment details, prescriptions, and medical procedures are accurately recorded in the billing system. Automated data transfer between clinical and financial records minimizes discrepancies and enhances workflow efficiency.
3. Automated Claim Processing
Claim management is a very essential aspect of medical billing, facilitated by AI-powered systems through automating claim submission, tracking, and error identification. Real-time claim validation helps healthcare providers decrease denials, accelerate reimbursement, and minimize labor. This feature simplifies hospital, insurance company, and patient transactions.
4. AI-Powered Medical Coding and Compliance Verifications
The use of efficient coding is essential in accurate billing and following health rules. AI helps in precise coding of diagnoses and procedures, minimizing error and regulatory compliance. Automated auditing also enhances precision by highlighting inconsistencies prior to claims submission, minimizing compliance risk and penalties.
5. Secure Payment Processing
Secure and reliable payment processing is essential to pure cash flow in medical billing. Multi-pay schemes are well-supported by AI systems and maintain data confidentiality and abide by industry rules such as HIPAA. The service improves patient satisfaction by simple, flexible, and uncomplicated payment processes.
6. Advanced Reporting and Analytics
AI facilitates end-to-end reporting and analytics to allow healthcare providers to monitor revenue, track billing trends, and determine areas to improve upon. With real-time information, healthcare organizations have the capacity to make data-driven decisions to improve financial performance, eliminate operational inefficiencies, and increase overall revenue management cycle.
Implementation Steps of AI in Medical Billing
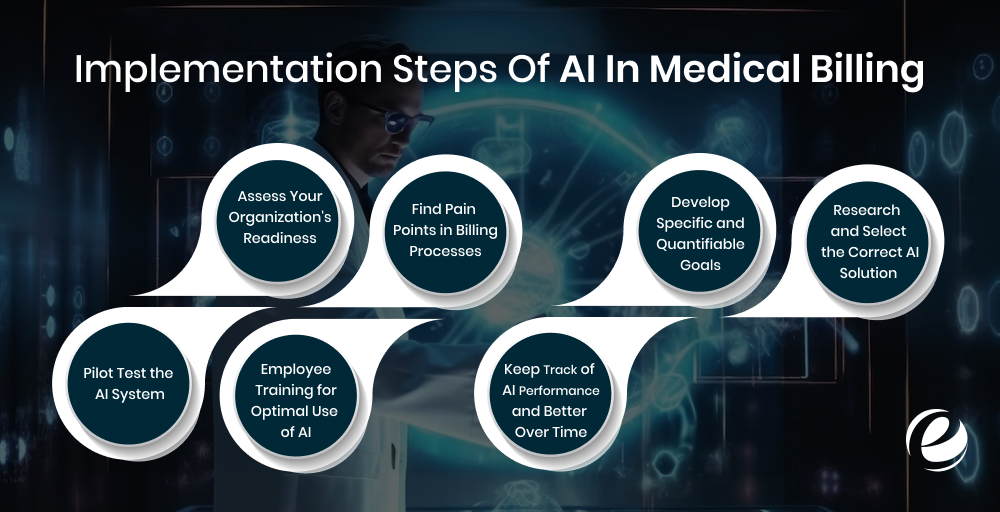
Artificial intelligence is revolutionizing medical billing with more accuracy, fewer errors, and quicker turnaround. There is a process, though, to effective implementation. Map the step-by-step plan for the successful integration of AI in your billing process.
#Step1. Assess Your Organization’s Readiness
Take a step back before implementing AI and ask yourself if your organization is ready for such a change. Look into your existing billing processes, IT infrastructure, and data management practices. Ask yourself the following:
- Is your billing process electronic or manual?
- Do you possess data structured in a way that the AI can efficiently process it?
- How technologically adept are your employees with respect to digital billing software?
A proper readiness assessment will reveal gaps and ensure the transition is made smoother while implementing new AI-based solutions.
#Step2. Find Pain Points in Billing Processes
AI performs optimally when applied where there is a scope for optimization. Go through your medical billing processes to identify inefficiencies, including:
- Persistent denial of claims due to improper coding
- Timely approval and reimbursement of claims
- Too much manual effort in data entry and processing
- Troubles in detecting fraud and compliance management
Identifying these inefficiencies, you can target AI solutions that will yield the highest return in efficiency and bottom line.
#Step3. Develop Specific and Quantifiable Goals
After identifying areas where AI can assist, develop specific and quantifiable goals. These are what will measure the success of AI. Some possible goals are:
- Decreasing the error rate in billing by 50% in six months
- Streamlining at least 80% of claim files
- Enhancing claim approval rates and decreasing the number of denials
- Monitor compliance to avoid penaltie
Clear-cut objectives will guide implementation of AI aligns with your company objectives.
#Step4. Research and Select the Correct AI Solution
There are multiple AI-based billing options available in the market today. Selecting the correct one is important. Research AI providers on the basis of the following factors:
- Shown track record for healthcare billing
- Ability to be used with your existing billing program
- Capacity for integrating with electronic health records (EHR)
- Security and compliance with regulations such as HIPAA
- Customer care and training facilities provided
Request product demos and case studies from potential vendors to understand how their solutions have helped similar healthcare organizations.
#Step5. Pilot Test the AI System
Before fully integrating AI, conduct a pilot test to evaluate its performance in a real-world setting. The trial phase should focus on:
- AI’s ability to accurately code and process claims
- Reduction in billing errors and processing time
- Seamless integration with existing systems
- User-friendliness and adaptability for staff
At this phase, take feedback from billing personnel in order to make the required modifications. Take feedback past any integration issues to achieve smooth implementation.
#Step6. Employee Training for Optimal Use of AI
Use of AI is as optimal as the staff using it. Give your billing staff thorough training on the use of AI-based technology. Training should encompass:
- Recovering AI-auto billing data
- Validating and verifying AI-recommended coding
- Fixing AI-identified claim issues
- Performing billing regulation upkeep
Continuous training and assistance will allow employees to use AI to its maximum potential, simplifying the entire process and making it better for accuracy.
#Step7. Keep Track of AI Performance and Better Over Time
Once installed, keep track of AI performance periodically to make sure that it is producing anticipated results. Keep a track of primary performance indicators (KPIs) such as:
- Rates of error reduction
- Reimbursement and claim approval time
- Effect of AI on revenue cycle performance
- Reduction in employees’ workload
Real-time monitoring will also enable constant fine-tuning of the system and AI algorithms so it can be updated with current billing regulation and industry trends.
Cost of Implementing AI in Medical Billing
The cost of deploying AI for medical billing varies based on various considerations including the nature of the AI model being deployed, the extent of automation needed, and how it integrates with the existing healthcare app. Whereas AI holds the potential for much higher efficiency & accuracy, the initial app development investment depends on specific needs.
The following is a general breakdown of some of the type of AI Applications and features involved in applying AI to medical billing:
| Type of AI Application | Estimated Cost Range | Features Included |
| Basic AI-Powered System | $10,000 – $50,000 | Does basic billing, checks insurance information, and minimizes human error. |
| Average AI-Integrated System | $50,000 – $150,000 | Has claim management, predictive analytics, and basic machine learning for error detection. |
| Advanced AI-Driven Application | $150,000 – $500,000+ | Leverages deep learning, automated coding, real-time claims tracking, and EHR seamlessly integrated. |
Use Cases of AI in Medical Billing
Artificial intelligence is revolutionizing medical billing by facilitating quicker, more accurate, and extremely efficient procedures. AI-based solutions automate the claims, detect fraud, and as well as revenue cycle management for medical professionals. A few of the basic applications of AI in medical billing are discussed below.
1. Detection and Prevention of Fraud
AI detects fraudulent billing patterns by checking massive volumes of data for out-of-sequence patterns. AI can stumble on repeat payments, unauthorized service stage improvement, and coding irregularities that include predictive fraud claims. AI can adapt to changing fraud strategies through ongoing learning, permitting providers to stay one step ahead of newly growing threats.
2. Increase Patient Billing Accuracy
With machines gaining knowledge of AI, patients are billed accordingly and accurately. AI checks bills are generated with proper treatment records, insurance, and payment terms. AI can even provide automated payment reminders and real-time cost estimates in seconds instantly, avoiding confusion and billing disputes.
3. Optimizing Revenue Cycles with Predictive Analytics
Artificial intelligence analysis helps predict late payment, claims denial, and loss of income based on historical billing trends and payer trends. This allows healthcare providers to take proactive action to maximize cash flow and reduce financial uncertainty, leading to enhanced financial management.
4. Reducing Claim Denials and Increasing Approvals
AI assists in determining the most common causes for claim denial and assists healthcare professionals in correcting the necessary issues before submitting. With denial trends being monitored in the long term, AI can recommend claim improvement, with faster approvals and little revenue loss.
Future of AI in Medical Billing

Artificial intelligence will transform medical billing into more precise, efficient, and secure processes. With improved automation, predictive analytics, and compliance management, AI-based solutions will enable healthcare providers to minimize errors, accelerate billing cycles, and enhance financial stability. Let us talk about some of the most important trends that are going to define the future of AI in medical billing.
1. Smarter Revenue Forecasting using AI
Artificial Intelligence analysis will allow medical professionals to predict the revenue cycle more accurately. AI, based on previous billing information and payment history, will be capable of identifying trends, projecting reimbursements, and helping organizations better manage their cash flows. It will reduce uncertainty around finances and help in overall revenue planning.
2. Security Upgrade with AI and Blockchain
With blockchain and AI integration, billing will be transparent and secure. AI detects billing discrepancies, and blockchain renders data tamper-proof and consistent. With these technologies combined, fraud claims will reduce, billing complaints will reduce, and payers’ trust in providers will increase.
3. Simplification of Repetitive Tasks through AI-Driven RPA
Artificial Intelligence (AI) enabled Robotic Process Automation (RPA) will mechanize painstaking billing processes like claim submissions, invoice issuances, and follow up on payment. Automation of such recurring operations will help health care organizations to reduce mistakes, accelerate payment processing, and free employees from administrative tasks so they can care for patients.
4. AI for Regulation and Compliance Management
Billing rules are constantly evolving, and AI will be an essential part of keeping providers compliant. AI-based software will track legal changes, payer policies, and billing codes for compliance threats. This forward-thinking strategy will enable healthcare providers to avoid penalties, minimize claim denials, and remain current with industry standards.
Why Choose EmizenTech for Implementation of AI in Medical Billing?
EmizenTech is a reputable brand in AI development, assisting healthcare practitioners in streamlining their billing process with smart and effective digital solutions. Our experience in healthcare software ensures that we provide customized platforms according to industry requirements and increase operational efficiency.
1. A Team of Experienced Professionals
Our worldwide team combines technology innovation, technical capability, and expertise areas. We specialize in creating AI-powered healthcare solutions for robotic billing and enhanced accuracy, freeing more time for the physicians to serve the patients.
2. A Legacy of Successful Projects
With more than thousands of projects delivered successfully across various industries, our reputation is known by all. Our work is in close collaboration with customers to create AI solutions that increase revenue cycle management, minimize errors, and streamline payment processing.
3. A Transparent and Efficient Development Approach
We follow a customer-centric approach with transparency at each phase of development. From consultation to deployment, we focus on timely delivery and tailored solutions for meeting the special needs of healthcare operations and medical billing.
4. Awards for Innovation and Excellence
Our innovation drive has also resulted in receiving extremely high-profile awards. These are the result of our dedication to innovating new horizons of AI-based healthcare solutions.
Conclusion
Artificial intelligence is revolutionizing the medical billing process by getting rid of errors, automating tasks, and simplifying finance operations for health practitioners. Through closing loopholes in the form of the manual recording of insurance claims and checks, and likely billing errors, AI greatly minimizes administrative work. This not only quickens reimbursement cycles, but it also ensures peak accuracy, permitting healthcare centers to devote less time to the detail of billing and more to taking care of patients.
But compliance with the regulations, data protection, and backward compatibility remain the primary issues. Despite all the issues, AI-powered billing software has long-term benefits that stretch from cost savings to process enhancement. AI in medical billing is a step for the future that can automate the workload and boost revenues. Join hands with EmizenTech to leverage the potential of AI and streamline your medical billing processes.
FAQs
How long is it to deploy AI in medical billing?
Project duration depends on the complexity of projects. 6–9 months can be dedicated to creating a Minimum Viable Product (MVP), but an end-to-end integrated system of AI will take more than one year. It takes sufficient time for every phase, such as data acquisition, training, testing, and deployment, so that it gets fine-tuned and enhanced to make it precise and efficient.
Can medical billing experts be fully substituted by AI?
Most of the medical billing activities such as coding and processing claims can be streamlined with the help of AI to the degree that the work for humans diminishes and makes errors obsolete. Full replacement soon is not feasible. Human cognitive abilities are still required for evaluating unusual conditions, dealing with complicated cases, and complying with ongoing healthcare regulations. AI is like a best-of-all-worlds solution, optimized productivity without outright replacing experts.
Is AI-based medical billing cost-effective?
AI-based medical billing can effectively save significant amounts by reducing manual effort and administrative costs. Errors eliminated due to automation reduce claim denials subsequently and increase reimbursement rates. Additionally, faster processing improves cash flow for healthcare professionals, making it a good investment in the long run.
How do we move from paper claims to total automation?
Migration from a paper-based to an entirely automated system is a gradual process. It starts with the scanning of existing records using Optical Character Recognition (OCR) technology. Artificial intelligence-based algorithms are trained on such data for processing and analysis. Automation with human oversight has to be performed for the first implementation in order to maintain accuracy. After optimal tuning of the system, medical practitioners can shift to a completely automated billing and coding system with very little manual intervention.